Although less than half the U.S. population has been fully immunized against COVID-19, medical experts and vaccine specialists are studying and preparing for the need for COVID-19 booster shots. Here’s a rundown of some of the big questions and answers – many of them tentative, as it’s still early days – having to do with coronavirus booster shots.
How long do coronavirus vaccines stay effective?
Both the Moderna and the Pfizer vaccines, which have accounted for more than 95% of U.S. vaccinations so far, remain highly effective for at least six months after the second shot. That’s based on the companies’ April announcements based on vaccinations among clinical-trial participants who received their first shots in summer 2020. As of early May 2021, Johnson & Johnson, maker of the third COVID-19 vaccine that has been granted U.S. Food and Drug Administration emergency authorization in the United States, had not disclosed data on longer-term effectiveness.
Will these vaccines’ effectiveness wane over time?
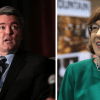
No one knows yet, says Dr. Thomas Campbell, a University of Colorado School of Medicine and UCHealth virologist and infectious-disease specialist. Campbell, who leads the Colorado portion of the Moderna COVID-19 vaccine clinical trial (217 people were enrolled locally of more than 30,000 nationally), says there’s no evidence so far that immunity conveyed by the Pfizer and Moderna vaccines is waning. But time will tell. Some vaccines, such as those for measles, last a lifetime. Others, such as flu vaccines, require annual updates – though in the case of flu vaccines, these “boosters” are designed to target new mutations of a fast-evolving virus.
Would COVID-19 booster shots be needed because the immune response from initial vaccination weakens over time – or, as in the case of flu vaccines, because the SARS-CoV-2 virus mutates in ways that render the vaccines less effective – or entirely ineffective?
Either/or – or both. The weakening of initial vaccine-based immunity over time, the potential of viral variants to render coronavirus vaccines less effective, or a combination of the two could trigger the need for COVID-19 booster shots, Campbell says.
“I think there’s a good chance that boosters will be needed,” he says, “but we don’t know how often they’ll be needed.”

The need for boosters and their frequency, he says, will depend on the ultimate longevity of the initial doses – still an open question – and whether viral variants emerge that can dodge today’s vaccines.
How effective are today’s vaccines against the current crop of coronavirus variants?
In laboratory studies, the Moderna and Pfizer vaccines are both highly effective in combatting the B.1.1.7 (British) variant of the virus. Other lab research has shown somewhat diminished effectiveness against the B.1.351 (South African) and P.1 (Brazilian) variants. It’s important to note, though, that the observation of antibody reactions in petri dishes doesn’t always translate into real-world immune responses. The Pfizer vaccine – whose protein-encoding mRNA is identical to Moderna’s – was effective in clinical trials in South Africa where B.1.351 was the dominant strain.
B.1.1.7 is now the dominant SARS-CoV-2 strain in the United States. Campbell says about 80% of new coronavirus cases nationally and roughly 70% of new Colorado cases involve coronavirus variants. The far greater transmissibility of certain variants of concern – the B.1.1.7 variant, for example, is believed to spread about 60% more easily and cause about 60% worse disease – has led to their growing dominance over previous versions of the virus.
Given the improbability of reaching herd immunity, the virus will continue to have opportunities to mutate, and there’s no guarantee that variants capable of dodging the current crop of vaccines won’t emerge. Indeed, as increasing numbers of people are fully vaccinated, a viral variant capable of evading vaccine protection, should one emerge, would find fertile ground among the vaccinated majority.
How are vaccine producers responding to the threat of variants and the possibility of diminishing vaccine-driven immunity over time?
Moderna officials say they’ll have COVID-19 booster shots ready by this fall. Pfizer officials also expect booster shots to be needed – and that such shots could boost antibody response (the body’s initial reaction to invading coronaviruses) by a factor of 10 or even 20. Both Pfizer and Moderna are already giving COVID-19 booster shots to a subset of their clinical-trial participants, and Pfizer, Moderna, and Johnson & Johnson are working on boosters tailored to the P.1.351 and other coronavirus variants.
These sorts of preparations make sense, Campbell says.
“SARS-CoV-2 is not going to go away,” he says. “In my opinion, it’s not going to be like measles, where we don’t have cases anymore.”
If COVID-19 booster shots are needed, can those initially vaccinated with Moderna get a Pfizer booster or vice-versa?
Probably, Campbell says. “Their delivery systems are a little bit different, but the Moderna and Pfizer vaccines create identical antigens,” he says, so the COVID-19 booster shots should be interchangeable.
Editor’s Note: During the pandemic, the Colorado Times Recorder will occasionally post articles, like this one, from UCHealth Today, which is published by UCHeatlh, the hospital associated with the University of Colorado School of Medicine. Our goal is to provide as many people as possible with accurate information about the virus and related topics.