By Rae Ellen Bichell, Kaiser Health News
Caitlin Wells Salerno knew that some mammals — like the golden-mantled ground squirrels she studies in the Rocky Mountains — invest an insane amount of resources in their young. That didn’t prepare her for the resources the conservation biologist would owe after the birth of her second son.
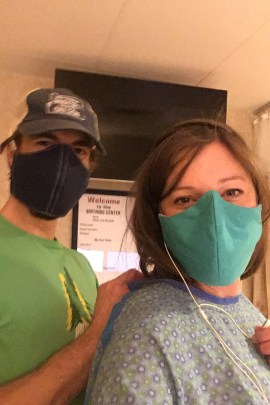
Wells Salerno went into labor on the eve of her due date, in the early weeks of coronavirus lockdowns in April 2020. She and her husband, Jon Salerno, were instructed to go through the emergency room doors at Poudre Valley Hospital in Fort Collins, Colorado, because it was the only entrance open.
Despite the weird covid vibe — the emptiness, the quiet — everything went smoothly. Wells Salerno felt well enough to decline the help of a nurse offering to wheel her to the labor and delivery department. She even took a selfie, smiling, as she entered the delivery room.
“I was just thrilled that he was here and it was on his due date, so we didn’t have to have an induction,” she said. “I was doing great.”
Gus was born a healthy 10 pounds after about nine hours of labor, and the family went home the next morning.
Wells Salerno expected the bill for Gus’ birth to be heftier than that for her first child, Hank, which had cost the family a mere $30. She was a postdoctoral fellow in California with top-notch insurance when Hank was born, about four years earlier. They were braced to pay more for Gus, but how much more?
Then the bill came.
The Patient: Caitlin Wells Salerno, a conservation biologist at Colorado State University and a principal investigator at Rocky Mountain Biological Laboratory. She is insured by Anthem Blue Cross Blue Shield through her job.

Medical Service: A routine vaginal delivery of a full-term infant.
Total Bill: $16,221.26. The Anthem BCBS negotiated rate was $14,550. Insurance paid $10,940.91 and the family paid the remaining $3,609.09 to the hospital.
Service Provider: Poudre Valley Hospital in Fort Collins, Colorado, operated by UCHealth, a nonprofit health system.
What Gives: In a system that has evolved to bill for anything and everything, a quick exam to evaluate labor in a small triage room can generate substantial charges.
The total bill was huge, but what really made Wells Salerno’s eyes pop was a line for the highest level of emergency services. It didn’t make any sense. Was it for checking in at the ER desk, as she’d been instructed to? She recalls going through security there on her way to labor and delivery, yet there was a $2,755 charge for “Level 5” emergency department services — as if she had received care there like a patient with a heart attack or fresh from a car wreck. It is the biggest item on the bill other than the delivery itself.
Dr. Renee Hsia, a professor of emergency medicine and health policy at the University of California-San Francisco and a practicing ER doctor, said Level 5 charges are supposed to be reserved for serious cases — “a severe threat to life, or very complicated, resource-intense cases” — not for patients who can walk through a hospital on their own. Emergency room visits are coded from Level 1 to Level 5, with each higher level garnering more generous reimbursement, in theory commensurate with the work required.
But over the past 20 years, hospitals and doctors have learned there’s great profit in upcoding visits. After all, the insurer isn’t in the exam room to know what transpired. An investigation by the Center for Public Integrity found that between 2001 and 2008 the number of Level 4 and 5 visits for patients who were sent homefrom the ER nearly doubled to almost 50% of visits. In Colorado, the Center for Improving Value in Health Care looked at emergency visit billing from 2009 to 2016 and found that the percentage of emergency visits coded as Level 5 steadily grew from 23% to 34% for patients with commercial insurance.
After repeated calls questioning the line item on her bill, Wells Salerno eventually got a voicemail from the billing department, which she shared with KHN, explaining that “the emergency room charge is actually the OB triage little area before they take you to the labor and delivery room.”
A customer service representative later explained it was for services given there when a nurse placed an IV for antibiotics, and her doctor checked her dilation and confirmed her water had broken — although none of that was performed in the Emergency Department. And those services, performed before every delivery, are traditionally not billed separately — and are routine, not emergency, procedures.
Some hospitals provide that package of services via an “obstetrical emergency department.” OB-EDs are licensed under the main Emergency Department and typically see patients who are pregnant, for anything from unexplained bleeding to full-term birth. They bill like an ER, even if they aren’t physically located anywhere near the ER.
Health care staffing company TeamHealth — owned by the investment company Blackstone, and known for marking up ER bills to boost profit — essentially says an OB-ED can be as simple as a rebranded obstetrical triage area. In a white paper, the company said an OB-ED is an “entrepreneurial approach to strengthening hospital finances” because with “little to no structural investment” it allows hospitals to “collect facility charges that are otherwise lost in the obstetrical triage setting.”
The OB Hospitalist Group, which is owned by a private equity company, markets a tool to help OB-EDs calculate levels of emergency care. In a case study, OB Hospitalist Group reported that hospitals “leave a lot of money on the table” by billing OB-ED visits as Level 1 and 2 emergencies when they could be considered Level 4 emergencies.
An Arizona facility said its revenue increased $365,000 per quarter after turning their obstetric triage area into an OB-ED. Poudre Valley Hospital’s website doesn’t list “OB-ED” as part of the facility’s offerings, though UCHealth documents do reference OB-ED beds in other facilities.
KHN spoke with four other women who, after giving birth at Poudre Valley in 2020 and 2021, received ER charges on their bills after healthy births. They had no clue they had received emergency services. One wrote a warning note on Facebook to other area moms after getting a whopping charge — for the 10 minutes she spent in the triage room, while fully dilated and in active labor.
In Wells Salerno’s case, UCHealth and her insurer have an agreement that Anthem BCBS pays a lump sum for vaginal delivery, rather than paying for line items individually. “Being seen there in OB-ED did not impact this bill whatsoever,” said Dan Weaver, a spokesperson with UCHealth.
But in one of the other moms’ cases, it did: The hospital received $1,500 from the insurer for that charge, and the mom was on the hook for an additional $375 for coinsurance.
Ge Bai, a professor of accounting and health policy at Johns Hopkins University, said it’s a “questionable” billing practice, and one that can matter to those who don’t have the same kind of insurance as Wells Salerno, or have none at all.
Dr. Mark Simon, chief medical officer with OB Hospitalist Group, said OB-EDs can help women avoid being admitted to the hospital too early in labor, ensuring timelier, more appropriate care.
UCHealth’s Weaver said they can also help pregnant patients with actual emergencies like preterm labor, preeclampsia or vaginal bleeding get quick care from specialists available 24/7, often without having to be admitted to the hospital. But at hospitals like Poudre Valley, healthy women having healthy births also get routine “OB-ED” treatment, without their knowledge.
Weaver said the only time someone in labor would not go through the OB-ED — and therefore the only time they would not receive the emergency charge — is if they have a scheduled induction or cesarean section or are directly admitted from a provider’s office.
Hsia, the UCSF researcher and ER doctor, is unconvinced: “If they’re actually going to charge a special fee that you didn’t get directly admitted from your physician, that’s absolutely ridiculous.”
Wells Salerno’s “OB-ED” exam was performed by her clinician, but the OB-ED charge still showed up on her bill.

Resolution: After trying to determine that the charge wasn’t a mistake, Wells Salerno eventually threw in the towel and paid the bill.
“I was at a very vulnerable time during pregnancy and immediately postpartum,” she said. “I just felt like I had kind of been taken advantage of financially at a time when I couldn’t muster the energy to fight back.”
The fact that two healthy brothers could come with such different price tags isn’t surprising to Dr. Michelle Moniz. “There is no clinical reason that we have this level of variation,” said Moniz, assistant professor of obstetrics and gynecology at the University of Michigan and its Institute for Healthcare Policy and Innovation. Her research shows that people with private insurance pay anywhere from nothing to $10,000 for childbirth.
“You don’t get what you pay for,” said Wells Salerno, who maintains that — despite their price difference — both of her children are equally “awesome.”
Data from the Colorado Division of Insurance shows that Poudre Valley typically received about $12,000 for similar births in 2020, about 43% more than the typical Colorado hospital. So the more than $14,000 Wells Salerno and her insurer paid is very high.
The Takeaway: Anything in our health system labeled as an emergency room service likely comes with a big additional charge.
Expectant parents should be aware that OB-EDs are a relatively new feature at some hospitals. Ask whether your hospital has that kind of charge and how it will affect your bill. Ahead of time, ask both the hospital and your insurer how much the birth is expected to cost. In Colorado, the Center for Improving Value in Health Care offers a price comparison tool for common medical procedures, including vaginal delivery.
If you do require a genuine ER encounter, look at your bill to see how it was coded, Levels 1 to 5 — and protest if your visit was misrepresented. Ask, “Has this bill been upcoded?” You are the only one who knows how much time you spent with a medical provider and how much care was given. Here’s a chart that will help with the proper definition of each level.
Know that victory is possible. At least one mom won the battle and got the emergency charge removed from her Poudre Valley Hospital birth bill. It took hours on the phone with UCHealth, a lot of confidence and countless repetitions of the birth story — and how an emergency charge for a routine delivery just didn’t, and doesn’t, make sense.




