COVID-19 infections are surging again, so if you are feeling sick, it’s important to get tested as quickly as possible.
If you test positive and have underlying medical issues that make you more vulnerable to severe illness —like being 65 or older, being pregnant, obese or having a suppressed immune system —you should seek COVID-19 treatments immediately.
Back in the beginning of the pandemic, doctors had few treatments to help people who got sick with COVID-19.
But coronavirus care has come a long way since early 2020, and advice from doctors is clear now. Don’t suffer at home. If you test positive for COVID-19 and you’re in a high-risk group, call your doctor and get help as quickly as possible.
COVID-19 treatments for at-risk people who test positive
The newest COVID-19 treatments include monoclonal antibodies like bebtelovimab and an intravenous antiviral medication, remdesivir. Both work well against the newest omicron variants and subvariants, BA.2 and BA.1.1, and are considered equivalent in terms of efficacy. Doctors also can prescribe antiviral medications like paxlovid (also considered as good as treatment as remdesivir and monoclonal antibody therapies) and molnupiravir (not quite as good as the others but still better than nothing). There’s also a relatively new medication that can prevent immunocompromised people from getting COVID-19 in the first place. It’s called evusheld.
Of course, everyone should get vaccinated and boosted against COVID-19 to decrease the likelihood of getting sick in the first place. But as immunities wane and variants spread, people who are vaccinated can get sick. If you are vaccinated and boosted, you’re likely to get a milder case if you do get COVID-19. Still, it’s wise to be prepared and know about medications that can help if you get sick.
The newest COVID-19 treatments are so valuable because they help people recover faster. They also have proven to be highly effective at preventing hospitalizations and deaths for people at high risk for suffering a poor outcome if they get COVID-19. These people include those who are older, immunocompromised, pregnant and obese.
“It’s unbelievable,” infectious disease specialist Dr. Michelle Barron said of the progress in developing COVID-19 treatments so quickly. “I put this in the same realm as vaccines.
“I would never have imagined that we’d have so many therapies. It just shows how far we can go when we have a shared purpose and a high level of investment in public health,” said Barron, who is UCHealth’s senior medical director of infection prevention and control and a professor at the University of Colorado School of Medicine on the Anschutz Medical Campus.
Over 65 with COVID? Call your doctor for treatment options
Barron urges people not to delay in asking for help.
“The goal of these medications is to keep people out of hospitals. If you have these risk factors, there’s a real risk of getting sick,” Barron said.
“Anyone in doubt about whether they might qualify should check with their doctor. And don’t be concerned that you should save COVID-19 treatments for people who might be at higher risk because in fact, you may be one of those people,” Barron said.
Even if you don’t feel severely ill when you first get infected, your illness could worsen quickly. And those who use the newest treatments need to take them early in the course of the illness.
“The time is now,” said Barron. “At this point, the supplies of these medications, especially the oral options, are good. You shouldn’t feel guilty for taking these medications if you are qualified to receive them. Call your doctor right now if you have tested positive for COVID-19. That’s the whole point of these medications: to use them to keep people out of hospitals.”
Barron helps answer your top questions about the newest COVID-19 treatments and who should get them.
Who should get COVID-19 therapies?
Monoclonal antibodies and antiviral medications are recommended for people who test positive for COVID-19 who are:
- 65 or older.
- Overweight or obese: with a BMI of 26 or greater.
- Dealing with cancer, kidney, liver, lung or sickle cell disease.
- Diagnosed with dementia, diabetes, Down Syndrome, heart conditions, HIV infections, certain mental health conditions and tuberculosis.
- Current or former smokers.
- Organ transplant recipients.
- Stroke survivors.
- Dealing with substance use disorders.
“You can look up the criteria yourself or call your provider. Oral antivirals are widely available at pharmacies now,” Barron said.
If you had to choose between monoclonal antibody infusion versus intravenous remdesivir or an oral antiviral like, paxlovid, which one would you choose?
“All of the options are good,” Barron said. “Clinical studies have shown that paxlovid, monoclonal antibodies, and intravenous remdesivir are equivalent in terms of keeping individuals out of the hospital. The decision regarding which one your provider may recommend depends on which options are available where you live and what therapy is easiest to access. Doctors also consider which specific conditions a person has or which medications they may be taking.”
Are there antiviral pills that work to reduce the severity of a COVID-19 infection?
Yes. There are two prescription medications that doctors are using currently. One is made by Pfizer and is called paxlovid. Merck manufactured the second medication, and it’s called molnupiravir. Both medications help prevent the virus that causes COVID-19 from spreading and are most effective when given early in the disease course.
What is paxlovid (a combination of Nirmatrelvir and ritonavir) and when does it work?
Paxlovid is an oral antiviral medication. Patients get a prescription from their doctor and pick up the medication at a pharmacy. They then take the antiviral pills for five days. The supplies for paxlovid have improved in recent weeks with more local pharmacies carrying a supply. It is being distributed for free by the U.S. federal government.
How effective is paxlovid?
According to drug makers, paxlovid reduced the risk of hospitalization and death by 89%.
Are there side effects?
Yes. Some people complain of gastrointestinal side effects like diarrhea. But some people who get sick with COVID-19 also get gastrointestinal symptoms. So, it’s difficult to know whether the infection or the medication is causing the symptoms, Barron said.
How quickly do I need to get paxlovid?
In order for the medication to work, patients must receive it within five days of getting symptoms of COVID-19.
What is molnupiravir (also known as Lagevrio)?
Molnupiravir is another type of oral antiviral medication. It’s a drug made by Merck. The effectiveness has been lower. Studies showed it prevented hospitalization and death by about 40%. It is being distributed for free by the U.S. federal government.
What are the possible side effects of molnupiravir?
They include diarrhea, dizziness, and nausea.
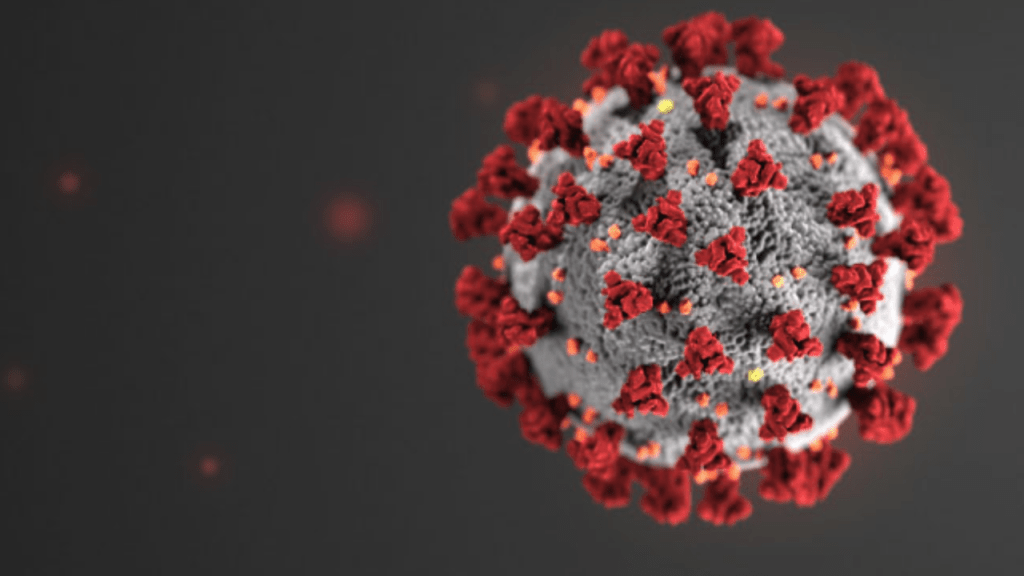
What are monoclonal antibodies?
Monoclonal antibodies are substances that experts manufacture in a lab that can specifically recognize and target the virus that causes COVID-19. These synthetic antibodies limit the ability of the virus to spread in the body. Monoclonal antibodies allow people to have a milder illness and thus, reduce hospitalizations and deaths.
How quickly do patients need to get monoclonal antibodies?
If you meet the criteria, it’s wise to get monoclonal antibodies as quickly after testing positive for COVID-19 as possible. The monoclonal antibodies will help patients as long as they receive them within seven days of symptom onset.
What is bebtelovimab?
Bebtelovimab is the newest version of monoclonal antibodies. It’s made by the pharmaceutical company, Lilly. It’s effective in combating the newest COVID-19 variants and sub variants. Read more about bebtelovimab.
How do I get bebtelovimab?
The U.S. government has spent $720 million for hundreds of thousands of doses of bebtelovimab that are being distributed around the country. For patients, the infusion is free (for now). If shortages occur, patients or insurance companies may need to foot the bill for monoclonal antibodies. (Review information about signing up for monoclonal antibodies through UCHealth.)
How long does it take to receive an infusion of monoclonal antibodies?
Patients go to a medical center and get an IV. Nurses then inject one dose of bebtelovimab into a person’s body through an IV. It only takes a few minutes to receive the medication, but nurses observe patients for at least an hour after the infusion to ensure that the patient is not having any side effects. Altogether an infusion appointment might take about two hours.
What are the possible side effects of bebtelovimab?
Side effects or allergies to monoclonal antibodies are rare and can include fever, difficulty breathing, low oxygen level in your blood, chills, tiredness, fast or slow heart rate, chest discomfort, wheezing, swelling of the lips, face, or throat, rash including hives, itching, muscle aches, dizziness, feeling faint, and sweating.
How many doses of bebtelovimab does a person need?
Patients receive a single dose of bebtelovimab.
What is remdesivir (Veklury)?
Remdesivir is an antiviral medication that patients receive via IV infusions. Drug maker Gilead developed remdesivir and Pfizer is manufacturing it in the U.S. Initially doctors used remdesivir to treat patients who were hospitalized for COVID-19. More recently, studies have shown that if patients receive remdesivir early in the course of their illness, they can avoid hospitalization.
How early in the course of the infection should a person get remdesivir?
It’s best to get the treatments as early as possible and within seven days of symptom onset.
How long does it take to receive an infusion of remdesivir?
The infusion time is short, but you will need to be observed for a period of time after the infusion, Barron said.
What are the possible side effects of remdesivir?
The most common side effect is nausea. Rarely, you can also have an allergic reaction or can also have an increase in your liver enzymes.
How many doses of remdesivir do people need?
Patients get three consecutive infusions.
What is evusheld?
It’s a medication for immunocompromised people who haven’t been able to produce enough antibodies after being vaccinated or for people that cannot get a COVID-19 vaccination due to an allergy or an allergic reaction to the vaccine. Evusheld, which is made by AstraZeneca, is a drug that immunocompromised people receive to prevent them from getting COVID-19.
Who should receive Evusheld?
- Patients who have received therapies in the last year that deplete B-cells. These include rituximab, ocrelizumab, ofatumumab and alemtuzumab.
- Patients receiving Bruton tyrosine kinase inhibitors.
- Recipients of chimeric antigen receptor T cells.
- Patients who have taken immunosuppressive medications.
- Patients with hematologic malignancies who are on active therapy.
- Lung transplant recipients.
- Patients who have received solid organ transplants within the last year.
- Other transplant patients who are dealing with acute rejection or those being treated with T or B cell depleting agents.
- Patients with severe combined immunodeficiencies
- Patients with untreated HIV.
How effective is evusheld?
People who received evusheld during clinical trials were 77% less likely to get COVID-19.
How many doses of evusheld should I get?
For now, doctors are recommending that people who need evusheld should receive a single dose.
How is evusheld administered?
“It is given as two consecutive intramuscular injections,” Barron said. “You will then be observed for up to an hour after administration.”
What are the side effects of evusheld?
You can have an allergic reaction after receiving the drug and also might have some soreness or bruising at the injection site.
Editor’s Note: During the pandemic, the Colorado Times Recorder will occasionally post articles from UCHealth Today, which is published by UCHeatlh, the hospital associated with the University of Colorado School of Medicine. Our goal is to provide as many people as possible with accurate information about the virus and related topics.




